Glioblastoma, also known as glioblastoma multiforme (GBM), is the most aggressive primary brain cancer in adults. It develops from glial cells, which support and protect neurons. Once formed, GBMs grow quickly and infiltrate nearby healthy tissue, making complete removal difficult. In the U.S., over 12,000 new GBM cases are diagnosed annually. Even with treatment, median survival is just 12–18 months, and just over 6 percent of patients survive five years or more.
What Makes Glioblastoma So Dangerous?
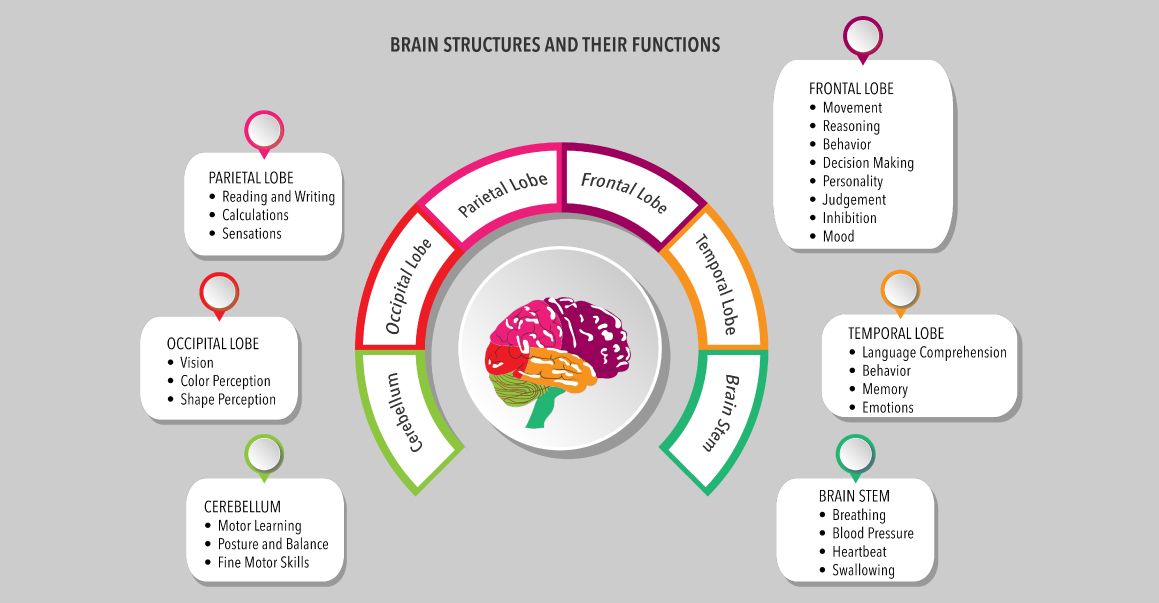
GBMs are highly invasive. The tumors spread microscopic tentacles into the healthy brain tissue, making it impossible to surgically remove the tumor cells completely. The tumor’s fast growth can also cause a range of neurological symptoms, depending on which part of the brain is affected. Common symptoms include persistent headaches, seizures, changes in memory or thinking, personality shifts, and trouble with speech or movement. Glioblastoma tends to return even after aggressive treatment; one of the reasons it is considered so difficult to manage.
Potential Risk Factors
Most cases have no clear cause, but certain factors are associated with higher GBM risk:
- Age: Most patients are over 50.
- Gender/Race: GBM is more common in males than females. Also, it is more prevalent in white individuals compared to Black, American Indian, Alaskan Native, and Asian-Pacific Islander populations.
- Genetic Conditions: Rare inherited disorders such as Li-Fraumeni syndrome, Turcot syndrome, and neurofibromatosis can elevate risk.
- Radiation Exposure: High-dose radiation to the head, typically from prior medical treatments, increases risk.
However, in most cases, the exact cause of glioblastoma is unknown. It does not usually run in families and lifestyle factors like diet, cell phone use, or environmental toxins have not been definitively linked to GBM.
Current Standard Treatments
The main therapies for GBM include:
- Surgery: to remove as much tumor as safely possible
- Radiation Therapy: usually around 60 Gray aimed at targeted areas. Gray or Gy is the unit used to measure the total amount of radiation that the patient is exposed to
- Chemotherapy: primarily temozolomide, which interferes with tumor DNA and slows growth
Despite aggressive treatment, GBMs typically recur within months, highlighting the need for research to develop innovative approaches.
Cold Plasma Therapy: A Game-Changer from GWU
One exciting development is cold plasma therapy, a novel treatment pioneered by Michael Keidar, PhD, and his team at the George Washington University. Cold plasma is an ionized gas at room temperature. Keidar, an aerospace engineer turned biomedical innovator, adapted plasma science from rocketry to medicine. His handheld device emits a stream of charged particles that generate reactive oxygen and nitrogen species (ROS and RNS). These species can selectively kill cancer cells while sparing healthy ones.
The Keidar Lab Team: Anmol Taploo, PhD, Vikas Soni, PhD, and Michael Keidar, PhD
In lab tests, GBM cells exposed to cold plasma underwent rapid DNA damage and their nuclei fragmented and cells died within minutes. Healthy cells showed minimal damage. Graduate student Vikas Soni discovered that cold plasma releases not only charged particles but also electromagnetic waves. These waves penetrate bone and skin to stimulate cancer cells to produce lethal levels of ROS/RNS, even through the skull. In mice with brain tumors, cold plasma treatment reduced tumor size without damaging surrounding tissue, demonstrating noninvasive penetration through bone.
Recently his team demonstrated the enhancement therapeutic efficacy of standard care drug Temozolomide (TMZ) via using a cold plasma source based on nonequilibrium plasma in a sealed glass tube, named a radial cold plasma discharge tube (PDT). The PDT affected glioblastoma cells’ function just by its electromagnetic (EM) emission rather than any chemical factors in the plasma. The PDT selectively increased the cytotoxicity of TMZ on two typical glioblastoma cell lines, U87MG and A172, compared with normal astrocyte cell line hTERT/E6/E7 to some extent. Furthermore, on the basis of a patient-derived xenograft model, this preliminary in vivo study demonstrated the drastically improved mean survival days of the tumor-barrier mice by more than 100% compared to control.
In 2015, a “light-saber-like” wand was used successfully during surgery on a colon cancer patient. Post-operative biopsies confirmed cancer cell destruction without harming normal tissue. A Phase I human clinical trial led by US Medical Innovations (USMI) and conducted at Rush University and Sheba Medical Center tested cold plasma on 20 patients with advanced solid tumors. The study confirmed safety and showed that treated tumor areas rarely experienced regrowth.
Keidar’s team is now developing a second, enclosed version of their cold plasma device that uses solely electromagnetic waves. This version is easier to use during surgery and in external brain treatments. With funding from the NSF’s I-Corps program and in collaboration with Duke University, they are preparing for clinical trials targeting glioblastoma.
Neurosurgeons are particularly hopeful. Cold plasma could be used to eliminate residual cancer cells around a tumor cavity without damaging normal brain tissue, potentially preserving vital functions.
Why This Matters
Glioblastoma remains one of the most formidable cancers. Its resistance to therapy and rapid recurrence make patient survival rates among the lowest. While cold plasma therapy is still experimental, it offers:
- Selective targeting of tumor cells
- Noninvasive delivery — even through bone
- Ability to combine with other treatments
If clinical trials confirm its safety and efficacy, cold plasma could revolutionize how GBM is treated, reducing recurrence and improving patient outcomes. Current therapies for glioblastoma aim to control growth, but rarely prevent relapse. Keidar’s cold plasma approach brings hope for more precise, less invasive, and more effective treatment. This breakthrough underscores the power of interdisciplinary research at the GW Cancer Center and the potential to bring new hope to patients, especially when hope has long been out of reach.



